Table of Contents
Introduction To Gut Inflammation And Mental State
Are you aware of the surprising connection between gut inflammation and mental state? Research has shown that the health of our gut plays a significant role in our overall well-being, including our mental health. In this article, we will explore the fascinating relationship between gut inflammation and our mental state, shedding light on how an unhealthy gut can impact our mood and cognitive function. So, let’s dive into the world of gut inflammation and its profound effects on our mental well-being.
In recent years, scientists have discovered that the gut, often referred to as our “second brain,” is closely linked to our mental health. The gut houses trillions of bacteria, collectively known as the gut microbiota, which play a crucial role in various bodily functions, including digestion, immune system regulation, and even the production of neurotransmitters that influence our mood.
When the delicate balance of the gut microbiota is disrupted, it can lead to gut inflammation. This inflammation, often caused by factors such as poor diet, chronic stress, or certain medications, triggers a cascade of events that can impact our mental state. Studies have found that individuals with gut inflammation are more likely to experience symptoms of anxiety, depression, and cognitive impairment.
The gut-brain axis, a bidirectional communication system between the gut and the brain, plays a vital role in this connection. When the gut is inflamed, it sends signals to the brain via various pathways, including the immune system, the vagus nerve, and the release of inflammatory molecules. These signals can disrupt the delicate balance of neurotransmitters in the brain, leading to mood disturbances and cognitive dysfunction.
Understanding the link between gut inflammation and our mental state opens up new possibilities for managing mental health conditions. By addressing gut health and reducing inflammation, we can potentially alleviate symptoms of anxiety and depression and improve cognitive function.
In upcoming articles, we will delve deeper into the specific mechanisms through which gut inflammation affects mental health and explore strategies to promote a healthy gut and support mental well-being. So, stay tuned as we unravel the fascinating connection between gut inflammation and our mental state, empowering you to take charge of your overall health and happiness.
Remember, taking care of your gut is not just about digestive health but also about nurturing a healthy mind. Let’s embark on this journey of understanding and optimizing our gut-brain connection for enhanced mental well-being.
What is Gut Inflammation?
Gut inflammation is a condition that occurs when the digestive tract becomes inflamed. It can be caused by a variety of factors, including poor diet, chronic stress, infections, and certain medications. The inflammation can occur in any part of the digestive tract, including the stomach, small intestine, and large intestine.
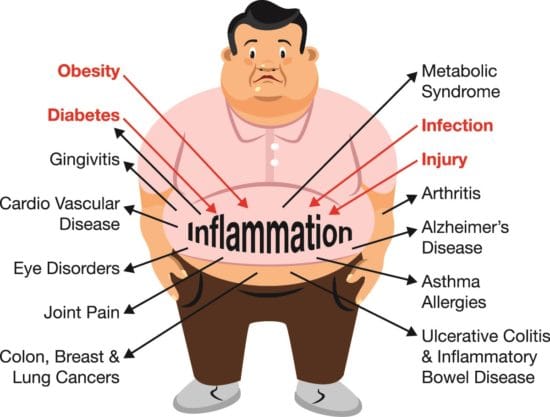
The inflammation process is a natural response of the immune system to fight off harmful substances, including bacteria and other pathogens. However, when the immune system is triggered continuously, it can lead to chronic inflammation, which can damage the tissues of the digestive tract and disrupt the gut microbiota.
The gut microbiota is a collection of microorganisms that live in the digestive tract. These microorganisms play a crucial role in maintaining gut health, including digestion, immune system regulation, and the production of essential nutrients and vitamins.

When the gut microbiota is disrupted due to inflammation, it can lead to various health problems, including inflammatory bowel disease (IBD), irritable bowel syndrome (IBS), and other digestive disorders. Symptoms of gut inflammation can include abdominal pain, bloating, diarrhea, constipation, and other digestive issues.
In addition to digestive problems, gut inflammation can also impact other areas of health, including mental health. Studies have shown that gut inflammation can contribute to the development of mental health conditions, including anxiety and depression.
To prevent gut inflammation, it is essential to maintain a healthy diet rich in fiber and nutrients, reduce stress levels, and avoid certain medications that can irritate the digestive tract. Probiotics and prebiotics can also help support a healthy gut microbiota and reduce inflammation.
Importance of Gut Health for Mental Well-being
Maintaining a healthy gut is crucial not only for digestion but also for our mental well-being. The gut, often referred to as the “second brain,” houses trillions of bacteria that form the gut microbiota. These bacteria play a vital role in various bodily functions, including the production of neurotransmitters that impact our mood and cognitive function.
The gut-brain connection is a bidirectional communication system between the gut and the brain. Research has shown that the state of our gut health can influence our mental state and vice versa. When our gut is healthy, it supports the production of neurotransmitters such as serotonin, dopamine, and gamma-aminobutyric acid (GABA), which are essential for regulating mood, reducing anxiety, and promoting overall mental well-being.
On the other hand, an unhealthy gut can lead to imbalances in these neurotransmitters, contributing to the development of mental health conditions such as anxiety and depression. Additionally, chronic inflammation in the gut can trigger systemic inflammation, which has been linked to mood disorders and cognitive decline.

The gut microbiota also plays a vital role in immune system regulation. A healthy gut microbiota helps to maintain a balanced immune response, preventing excessive inflammation that can negatively impact mental health. Imbalances in the gut microbiota, known as dysbiosis, have been associated with increased vulnerability to stress, anxiety, and depression.
Furthermore, the gut microbiota produces short-chain fatty acids (SCFAs), which are crucial for maintaining the integrity of the gut lining. A healthy gut lining acts as a barrier, preventing harmful substances from entering the bloodstream. When the gut lining is compromised, toxins and inflammatory molecules can leak into the bloodstream, leading to systemic inflammation and potential effects on mental health.
To support a healthy gut and promote mental well-being, it is important to focus on a few key factors. First and foremost, a balanced and nutritious diet is essential. Including fiber-rich foods, fruits, vegetables, and fermented foods can help nourish the gut microbiota. Probiotic-rich foods or supplements can also introduce beneficial bacteria to the gut.
Managing stress is another crucial aspect of promoting gut health and mental well-being. Chronic stress can disrupt the gut-brain axis and negatively impact the gut microbiota. Engaging in stress-reducing activities such as exercise, mindfulness, and adequate sleep can help maintain a healthy gut and support mental wellness
Types and Categories
Chronic vs. Acute Inflammation
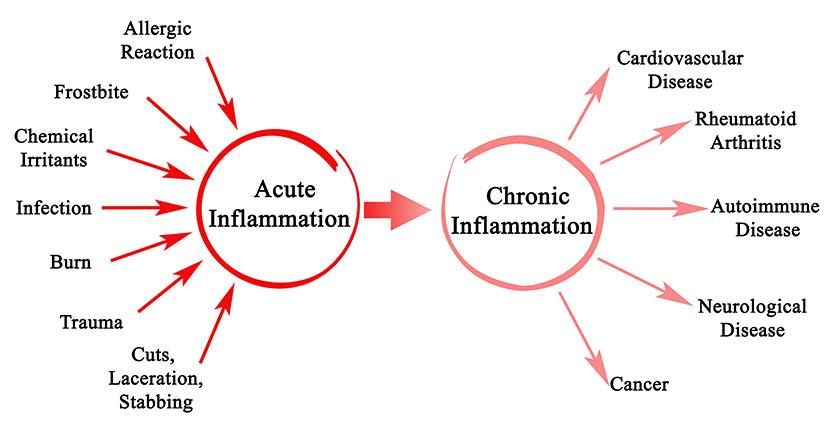
Inflammation is a natural response of the immune system to injury or infection. It is a vital process that helps the body fight off harmful agents and initiate the healing process. However, inflammation can be categorized into two types: chronic and acute, each with distinct characteristics and implications for our health.
Acute inflammation is a short-term response that occurs immediately after tissue injury or infection. It is characterized by symptoms such as redness, swelling, heat, and pain in the affected area. Acute inflammation is a protective mechanism that helps isolate and eliminate the source of injury or infection. It is typically self-limiting, meaning it resolves once the healing process is complete.
On the other hand, chronic inflammation is a long-lasting and persistent inflammatory response that can last for weeks, months, or even years. Unlike acute inflammation, chronic inflammation is not self-limiting and can result in tissue damage over time. It is often a result of an underlying health condition, such as autoimmune disorders, chronic infections, or prolonged exposure to irritants.
Chronic inflammation can occur throughout the body and has been linked to various health conditions, including cardiovascular disease, diabetes, arthritis, and certain types of cancer. Unlike acute inflammation, which is characterized by visible symptoms, chronic inflammation is often silent and may not present noticeable signs. Instead, it can manifest as low-grade inflammation that affects multiple systems in the body.
One of the key differences between chronic and acute inflammation is the immune response involved. Acute inflammation is primarily mediated by neutrophils, a type of white blood cell, while chronic inflammation involves the activation of immune cells such as macrophages and lymphocytes. This sustained immune response in chronic inflammation can lead to the release of pro-inflammatory substances, further perpetuating the inflammatory process.
The causes of chronic inflammation are multifactorial. Unhealthy lifestyle factors, such as poor diet, sedentary behavior, chronic stress, and obesity, can contribute to chronic inflammation. Environmental factors, such as exposure to pollutants or toxins, can also play a role. Additionally, underlying health conditions, such as autoimmune disorders or chronic infections, can trigger and perpetuate chronic inflammation.
Managing chronic inflammation is crucial for maintaining overall health and preventing the development of chronic diseases. Lifestyle modifications, including adopting a balanced and nutritious diet, engaging in regular physical activity, managing stress levels, and avoiding exposure to environmental toxins, can help reduce chronic inflammation. Additionally, certain anti-inflammatory foods and supplements, such as omega-3 fatty acids and turmeric, may provide additional support.
Specific Conditions: IBD, IBS, and Gastritis
Inflammatory Bowel Disease (IBD), Irritable Bowel Syndrome (IBS), and Gastritis are three distinct conditions that affect the gastrointestinal system. While they may share some similarities in symptoms, causes, and management, it is important to understand their unique characteristics.
IBD is an umbrella term that encompasses two main conditions: Crohn’s disease and ulcerative colitis. These are chronic inflammatory disorders that primarily affect the digestive tract. In IBD, the immune system mistakenly attacks the gastrointestinal lining, leading to inflammation and damage. Symptoms can vary but often include abdominal pain, diarrhea, rectal bleeding, weight loss, and fatigue. Treatment for IBD focuses on reducing inflammation, managing symptoms, and preventing complications through medication, lifestyle changes, and sometimes surgery.
IBS, on the other hand, is a functional gastrointestinal disorder. It is characterized by a group of symptoms that occur together, including abdominal pain, bloating, changes in bowel habits (such as diarrhea, constipation, or both), and relief of symptoms after passing stool. Unlike IBD, IBS does not cause inflammation or permanent damage to the digestive tract. The exact cause of IBS is unknown, but factors such as abnormal muscle contractions in the intestines, hypersensitivity to pain, and disturbances in the gut-brain axis may contribute. Treatment for IBS focuses on managing symptoms through dietary modifications, stress management techniques, and medications to alleviate specific symptoms.
Gastritis refers to inflammation of the stomach lining. It can be acute, occurring suddenly and lasting for a short duration, or chronic, persisting over an extended period. Gastritis can be caused by various factors, including infection with Helicobacter pylori bacteria, excessive alcohol consumption, long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), stress, and autoimmune disorders. Symptoms of gastritis may include abdominal pain, nausea, vomiting, bloating, loss of appetite, and indigestion. Treatment for gastritis depends on the underlying cause and may involve medications to reduce stomach acid, antibiotics for bacterial infections, lifestyle modifications, and avoiding triggers such as alcohol and NSAIDs.
While these conditions can cause discomfort and impact daily life, they can be managed with proper medical guidance and lifestyle adjustments. It is crucial to consult with healthcare professionals for an accurate diagnosis, personalized treatment plans, and ongoing management strategies. With the right approach, individuals with IBD, IBS, or gastritis can lead fulfilling lives while effectively managing their symptoms and promoting optimal gastrointestinal health.
Symptoms and Signs
Common Symptoms of Gut Inflammation
Gut inflammation refers to the inflammation of the gastrointestinal tract, which can occur due to various reasons such as infections, autoimmune disorders, or dietary factors. While the specific symptoms can vary depending on the underlying cause and individual differences, there are some common signs that indicate gut inflammation. Understanding these symptoms can help in identifying and managing gut inflammation effectively.
Abdominal pain is a prevalent symptom of gut inflammation. It may range from mild discomfort to severe cramping, and the location of the pain can differ based on the specific area of the gastrointestinal tract affected. Individuals may experience pain in the lower abdomen, upper abdomen, or throughout the entire abdominal region.

Bloating and distension are also common symptoms associated with gut inflammation. The abdomen may feel swollen or full due to excess gas production or impaired digestion. This can lead to discomfort and a sensation of heaviness.
Changes in bowel habits are often observed in individuals with gut inflammation. Diarrhea may occur, characterized by loose, watery stools and increased frequency of bowel movements. Conversely, constipation can also be a symptom, where individuals may experience difficulty in passing stools or have infrequent bowel movements.
Nausea and vomiting may occur in some cases of gut inflammation, particularly when the upper gastrointestinal tract is affected. This can contribute to a loss of appetite and a feeling of general malaise.
Blood in the stool is a significant symptom that should not be ignored. It can indicate inflammation or injury within the gastrointestinal tract. The presence of blood can range from visible red blood in the stool to dark, tarry stools, depending on the location and severity of inflammation.
Another common symptom of gut inflammation is fatigue. Chronic inflammation can lead to a persistent feeling of tiredness and low energy levels. This can be attributed to the body’s immune response and the energy required for the healing process.
In some cases, gut inflammation may also cause unintended weight loss. This can occur due to a combination of factors such as decreased appetite, malabsorption of nutrients, increased metabolic demands, and an overall inflammatory state.
Individuals with gut inflammation may experience food intolerances or sensitivities. Certain foods may trigger or exacerbate inflammation, leading to symptoms such as bloating, abdominal pain, and diarrhea. Identifying and avoiding these trigger foods can help manage symptoms effectively.
It is important to note that these symptoms can overlap with other gastrointestinal conditions, and a proper diagnosis is essential. If you experience persistent or worsening symptoms of gut inflammation, it is advisable to consult with a healthcare professional for an accurate evaluation and personalized treatment plan
Uncommon Signs to Watch Out For
While we are familiar with common signs and symptoms of various health conditions, it is equally important to be aware of the uncommon signs that may indicate underlying health concerns. These less frequently observed symptoms can provide valuable insights and prompt us to seek medical attention when necessary. Here are some uncommon signs to watch out for:
- Unexplained weight changes: Sudden and unexplained weight gain or loss may be indicative of an underlying health issue. It could be a result of hormonal imbalances, metabolic disorders, or even certain medications.
- Changes in skin appearance: Pay attention to any unusual changes in your skin. These may include persistent rashes, excessive dryness, discoloration, or the appearance of new moles or growths. Such changes could be a sign of skin conditions, allergies, or even skin cancer.
- Changes in urinary habits: If you notice any significant changes in your urinary habits, such as increased frequency, urgency, pain while urinating, or blood in the urine, it may be a sign of a urinary tract infection, kidney stones, or other urinary disorders.
- Persistent headaches: While occasional headaches are common, persistent or severe headaches that are not relieved by over-the-counter pain relievers may warrant medical attention. They could be a symptom of migraines, tension headaches, or underlying conditions like brain tumors or infections.
- Unusual fatigue or weakness: If you find yourself feeling excessively tired or experiencing unexplained weakness, despite getting enough rest, it may be worth investigating. Fatigue can be a symptom of various conditions, including anemia, thyroid disorders, chronic fatigue syndrome, or even psychological factors such as depression or anxiety.
- Changes in vision: Any sudden or significant changes in your vision should not be ignored. Blurred vision, double vision, or difficulty focusing may indicate eye problems, such as cataracts, glaucoma, or even neurological issues that require medical attention.
- Digestive abnormalities: Pay attention to any persistent or recurring digestive abnormalities, such as chronic indigestion, difficulty swallowing, or unexplained changes in bowel habits. These can be signs of gastrointestinal disorders, food intolerances, or even underlying issues like inflammatory bowel disease or certain cancers.
- Cognitive changes: Any unexplained or sudden changes in cognitive function, such as memory loss, confusion, difficulty concentrating, or personality changes, should be taken seriously. These symptoms may be indicative of neurological conditions, such as dementia, Alzheimer’s disease, or even a brain injury.
- Mood disturbances: Persistent changes in mood, such as prolonged feelings of sadness, irritability, hopelessness, or unexplained mood swings, may be signs of mental health conditions like depression, anxiety, or bipolar disorder. Seeking professional help can provide necessary support and guidance.
- Unusual pain or discomfort: If you experience unexplained or persistent pain or discomfort in any part of your body, it is important to have it evaluated. This includes unusual headaches, chest pain, joint pain, or abdominal pain that cannot be attributed to a known cause.
Causes and Risk Factors
Biological Factors Leading to Inflammation
- Genetics: Genetic factors can influence the body’s immune response to infections and other stimuli, leading to chronic inflammation. Certain genetic variations can increase the risk of autoimmune disorders, which are characterized by inflammation and damage to the body’s own tissues.
- Environmental factors: Exposure to environmental factors such as pollution, toxins, and infectious agents can trigger chronic inflammation. Air pollution, for instance, can cause lung inflammation, while exposure to certain toxins can lead to liver inflammation and damage.
- Diet: The food we eat can also influence inflammation levels in the body. Consuming a diet high in processed foods, saturated and trans fats, and sugar can lead to chronic inflammation. In contrast, a diet rich in fruits, vegetables, whole grains, and healthy fats can help reduce inflammation levels.
- Gut microbiome: The gut microbiome, which refers to the trillions of microorganisms living in our gut, plays a crucial role in regulating inflammation levels. An imbalance of the gut microbiome, known as dysbiosis, can lead to chronic inflammation and various health conditions.
- Hormones: Hormones such as cortisol and estrogen can modulate the immune response and inflammation levels in the body. An imbalance in hormone levels, such as during menopause or stress, can lead to chronic inflammation and related health issues.
- Chronic infections: Certain chronic infections, such as hepatitis B and C, HIV, and Lyme disease, can trigger chronic inflammation and damage to organs and tissues. These infections can also lead to autoimmune disorders, further exacerbating inflammation levels.
- Age: As we age, our immune system undergoes changes that can lead to chronic inflammation. Age-related inflammation, or inflammaging, is associated with various age-related diseases, including Alzheimer’s disease, osteoporosis, and cardiovascular diseases.
Environmental Triggers and Their Impact
- Air Pollution: Poor air quality, caused by pollutants from vehicles, industrial emissions, and other sources, can have detrimental effects on our respiratory system. Breathing in polluted air can lead to respiratory problems, such as asthma, bronchitis, and even lung cancer.
- Allergens: Allergens in the environment, such as pollen, dust mites, pet dander, and mold spores, can trigger allergic reactions in susceptible individuals. These reactions can manifest as respiratory symptoms, skin rashes, or even severe anaphylactic reactions.
- Chemical Exposure: Exposure to harmful chemicals in our surroundings, such as pesticides, cleaning agents, and industrial chemicals, can have adverse health effects. Prolonged or excessive exposure to these chemicals can lead to respiratory issues, skin allergies, hormonal imbalances, and even an increased risk of certain cancers.
- Noise Pollution: Excessive noise levels from traffic, construction sites, or industrial activities can impact our mental and physical well-being. Chronic exposure to high noise levels can lead to stress, sleep disturbances, hearing loss, and cardiovascular problems.
- Water Contamination: Contamination of water sources with pollutants, chemicals, or microorganisms can pose significant health risks. Consuming contaminated water can lead to waterborne diseases, gastrointestinal issues, and long-term health complications.
- Extreme Temperatures: Extreme heat or cold can have a direct impact on our health. Heatwaves can lead to heat exhaustion, heatstroke, and exacerbate cardiovascular conditions. Extreme cold can increase the risk of hypothermia, frostbite, and respiratory issues.
- Natural Disasters: Natural disasters like earthquakes, hurricanes, floods, and wildfires can cause widespread damage and have a profound impact on communities. They can lead to displacement, injuries, mental health issues, and the spread of diseases in affected areas.
- Light Pollution: Excessive artificial lighting at night can disrupt our natural sleep patterns and affect our overall health. It can lead to sleep disorders, hormonal imbalances, and an increased risk of obesity, diabetes, and certain cancers.
- Green Spaces: On the positive side, access to green spaces, such as parks and gardens, can have a beneficial impact on our well-being. Spending time in nature can reduce stress, improve mood, boost cognitive function, and enhance overall mental and physical health.
- Built Environment: The design of our built environment, including architecture, urban planning, and infrastructure, can influence our physical activity levels, access to amenities, and overall quality of life. Well-designed and walkable communities can promote active lifestyles and better health outcomes.
Lifestyle Choices Influencing Gut Health
- Diet: The food we eat has a direct impact on our gut health. A diet high in fiber from fruits, vegetables, whole grains, and legumes promotes a healthy gut. These foods are rich in prebiotics, which nourish beneficial gut bacteria. On the other hand, a diet high in processed foods, added sugars, and unhealthy fats can disrupt the balance of gut bacteria and contribute to digestive issues.
- Hydration: Staying adequately hydrated is essential for a healthy gut. Water helps to soften stools and supports proper digestion. It also aids in the absorption of nutrients from the food we consume. Drinking enough water throughout the day helps maintain optimal gut function.
- Physical Activity: Regular exercise has numerous benefits for our overall health, including gut health. Exercise helps to regulate bowel movements and promotes healthy digestion. It can also reduce stress levels, which can have a positive impact on the gut by minimizing gut-related symptoms like bloating and discomfort.
- Stress Management: Chronic stress can disrupt the balance of gut bacteria and contribute to digestive problems. Finding effective ways to manage stress, such as practicing mindfulness, engaging in relaxation techniques, or pursuing hobbies, can support a healthy gut. Prioritizing self-care and taking time to relax can have a positive impact on gut health.
- Sleep: Sufficient and quality sleep is essential for maintaining a healthy gut. During sleep, the body carries out important restorative processes, including gut repair and regulation of gut hormones. Poor sleep habits can disrupt these processes and lead to gut-related issues like inflammation and impaired digestion.
- Antibiotic Use: While antibiotics are necessary to treat bacterial infections, their overuse or misuse can disrupt the balance of gut bacteria. Antibiotics not only kill harmful bacteria but can also reduce beneficial bacteria. If prescribed antibiotics, it is crucial to follow the recommended dosage and consider probiotic supplementation or consume probiotic-rich foods to replenish the gut with beneficial bacteria.
- Alcohol and Smoking: Excessive alcohol consumption and smoking can negatively impact gut health. Alcohol can irritate the digestive system and disrupt the gut microbiome. Smoking can also harm the gut lining and increase the risk of digestive disorders. Minimizing alcohol intake and quitting smoking can contribute to a healthier gut.
- Medication Use: Certain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and proton pump inhibitors (PPIs), can affect gut health. Prolonged use of these medications can lead to gut irritation and an imbalance in gut bacteria. It is important to use medications as prescribed and consult with healthcare professionals about potential gut-related side effects.
Diagnosis and Tests
Diagnostic Tools: Endoscopy and Imaging Techniques
- Endoscopy: Endoscopy is a minimally invasive diagnostic tool that involves inserting a flexible tube with a camera and light attached to it into the body. This procedure allows physicians to examine the inside of the body, such as the digestive tract, respiratory system, and urinary system. Endoscopy can be used to diagnose conditions like ulcers, inflammation, tumors, and other abnormalities. It can also be used to take samples for further testing or to perform therapeutic interventions, such as removing polyps or treating bleeding.
- X-Ray: X-rays are a commonly used imaging technique that uses electromagnetic radiation to produce images of internal structures. This non-invasive technique can help diagnose a range of conditions, such as fractures, pneumonia, and tumors. X-ray is also used to monitor the progress of treatment and to guide certain surgical procedures.
- Ultrasound: Ultrasound is a non-invasive imaging technique that uses high-frequency sound waves to produce images of internal structures. It is commonly used to examine the abdominal and pelvic regions, as well as the heart and blood vessels. Ultrasound can help diagnose conditions like gallstones, tumors, and cysts. It can also be used to guide certain procedures, such as biopsies or fluid drainage.
- CT Scan: A CT (computed tomography) scan is an imaging technique that uses X-rays and computer technology to produce detailed cross-sectional images of internal structures. This procedure provides more detailed images than X-rays alone and is commonly used to examine the head, chest, abdomen, and pelvis. CT scan can help diagnose conditions like tumors, fractures, and internal bleeding.
- MRI: Magnetic resonance imaging (MRI) is a non-invasive imaging technique that uses a strong magnetic field and radio waves to produce detailed images of internal structures. It is commonly used to examine the brain, spine, joints, and soft tissues. MRI can help diagnose conditions like tumors, inflammation, and degenerative diseases.
- PET Scan: Positron emission tomography (PET) scan is a diagnostic tool that uses a radioactive substance to produce images of internal structures. This technique is commonly used to examine the brain, heart, and certain types of cancer. PET scan can help diagnose conditions like tumors, inflammation, and metabolic disorders.
Blood Tests and Biomarkers for Inflammation
- Complete Blood Count (CBC): A complete blood count (CBC) is a basic blood test that measures the number of red blood cells, white blood cells, and platelets in the blood. Elevated levels of white blood cells, specifically neutrophils, can indicate an inflammatory response. A CBC can also identify anemia, a condition that can contribute to chronic inflammation.
- C-Reactive Protein (CRP): C-reactive protein (CRP) is a biomarker that indicates the presence of inflammation in the body. High levels of CRP can indicate the presence of acute or chronic inflammation. CRP can be used to monitor the progress of treatment of diseases that involve inflammation, such as rheumatoid arthritis and inflammatory bowel disease.
- Erythrocyte Sedimentation Rate (ESR): Erythrocyte sedimentation rate (ESR) is a blood test that measures the rate at which red blood cells settle in a test tube. Elevated ESR levels can indicate an inflammatory response, but this test is less specific than CRP and can be influenced by other factors, such as anemia.
- Tumor Necrosis Factor (TNF): Tumor necrosis factor (TNF) is a cytokine that plays a crucial role in the inflammatory response. High levels of TNF can indicate the presence of inflammation and are associated with a range of inflammatory diseases, such as rheumatoid arthritis, psoriasis, and Crohn’s disease.
- Interleukin-6 (IL-6): Interleukin-6 (IL-6) is a cytokine that promotes inflammation and is associated with a range of inflammatory diseases. Elevated levels of IL-6 can indicate the presence of inflammation and can be used to monitor the progress of treatment for inflammatory conditions.
- Fibrinogen: Fibrinogen is a protein that plays a crucial role in blood clotting and wound healing. Elevated levels of fibrinogen can indicate the presence of inflammation and are associated with a range of inflammatory diseases, such as cardiovascular disease.
Read More : Best Foods that Boost Gut Health and Mental Well-being
Reference : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3065426/

